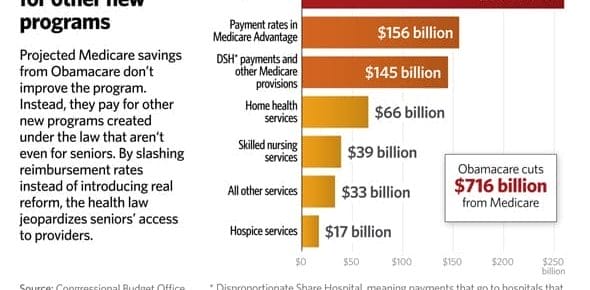
You are turning 65. What are the Medicare traps and mistakes most retirees make in navigating the Medicare maze? One wrong decision can cost you thousands of dollars. Your choice is much more …
5 Medicare Myths
We talk to a lot of Georgia seniors and find there are at least 5 Medicare myths that are common and should be addressed. If you fall prey to these Medicare myths you could end up paying more for your …