Does Medicare cover hearing tests and hearing aids? Find financial assistance to offset the cost of hearing exams and aids. How Veterans can get help for hearing and vision concerns. Purchase high …
AARP – Is It Worth It?
AARP membership is only $16, but is it worth it? What do you really get for your membership fee? How does AARP provider all these benefits for only $16? How is AARP funded? Are their discounts on …
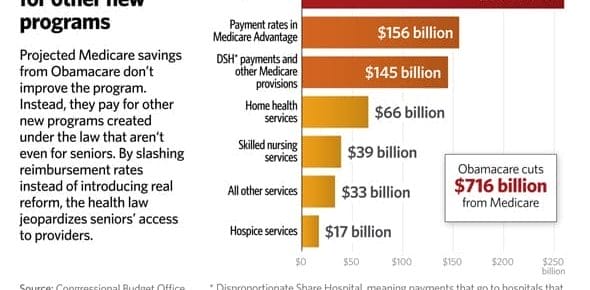
How Obamacare Impacts Medicare Advantage Plans
Obamacare affected under age 65 health insurance but left Medicare alone. That popular belief is incorrect. Obamacare (ACA) reduces funding for Medicare plans and cut's reimbursement to carriers. …
Continue Reading about How Obamacare Impacts Medicare Advantage Plans →
Proposed Medicare Changes Will Hurt Georgia Seniors
The DC spending monster is hungry and proposed Medicare changes means they expect Georgia seniors to feed them. Their solution calls for shared funding and shared responsibility. That translates into …
Continue Reading about Proposed Medicare Changes Will Hurt Georgia Seniors →
5 Medicare Myths
We talk to a lot of Georgia seniors and find there are at least 5 Medicare myths that are common and should be addressed. If you fall prey to these Medicare myths you could end up paying more for your …
Medicare Cuts Fund Obamacare
Georgia seniors will get a rude awakening in January when Medicare cuts fund Obamacare. You were warned. Obamacare is funded, at least in part, on the backs of seniors that rely on Medicare. Starting …